Medicare Savings Programs (MSPs) are a vital part of the support structure for low-income Medicare beneficiaries. These state-run programs are designed to help eligible individuals pay for out-of-pocket Medicare costs such as premiums, deductibles, coinsurance, and copayments associated with Medicare Part A and Part B. Understanding MSPs is essential for insurance agents working with seniors and disabled individuals, as enrollment can significantly increase the affordability and accessibility of healthcare. This module will introduce the four primary Medicare Savings Programs, outline eligibility requirements, and provide an overview of the benefits they offer. Agents will gain foundational knowledge that will allow them to identify qualifying clients and assist them in navigating enrollment, ensuring those most in need receive the financial support they deserve.

The Low-Income Subsidy (LIS), also known as Extra Help, is a federal program that helps Medicare beneficiaries with limited income and resources afford their Part D prescription drug costs. It reduces or eliminates monthly premiums, annual deductibles, and copayments based on three levels of eligibility tied to income and asset thresholds. Beneficiaries can qualify automatically through programs like Medicaid, SSI, or Medicare Savings Programs, or they can apply through the Social Security Administration or their state Medicaid office. LIS applies to both standalone drug plans (PDPs) and Medicare Advantage plans with drug coverage (MA-PDs), covering only formulary drugs and subsidizing premiums up to the state-specific benchmark amount. Understanding LIS is essential for identifying eligible clients, verifying their status, and helping them choose cost-effective plans that maximize their benefits.


Chronic Condition Special Needs Plans (C-SNPs) are specialized Medicare Advantage plans designed to provide tailored care, benefits, and prescription drug coverage for beneficiaries living with specific chronic illnesses such as diabetes, heart failure, and cardiovascular disorders. To enroll, individuals must be enrolled in Medicare Parts A and B, live in a plan’s service area, and have an official diagnosis verified by their doctor using a Verification of Chronic Condition (VCC) form within 60 days of enrollment. Agents play a vital role in identifying qualified clients by asking structured health screening questions and guiding them through documentation, objection handling, and enrollment. When offered appropriately, C-SNPs help clients receive condition-specific support, reduce hospitalizations, and improve long-term health outcomes.
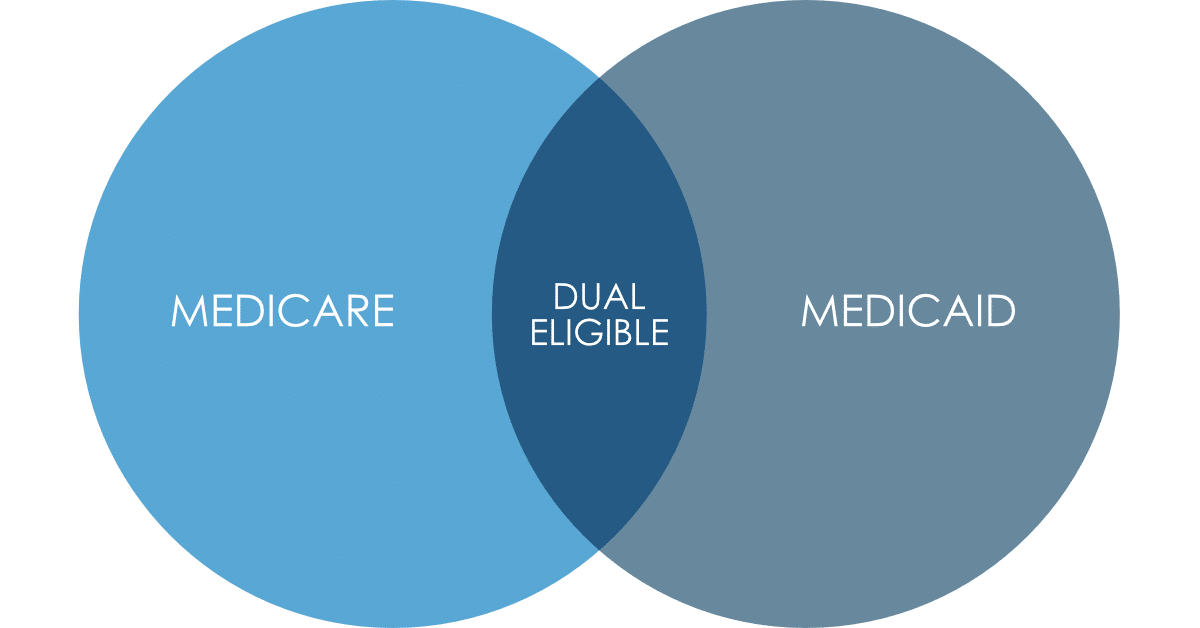
Dual Eligible Special Needs Plans (DSNPs) are specialized Medicare Advantage plans designed for individuals who qualify for both Medicare and Medicaid. These plans integrate the benefits of traditional Medicare with supplemental Medicaid services, providing tailored care coordination, enhanced benefits, and additional supports that address the complex health needs of dual eligibles. DSNPs offer comprehensive coverage that often includes vision, dental, hearing, transportation, and prescription drug benefits—services that might not be fully covered under standard Medicare or Medicaid alone. By consolidating services and simplifying access to care, DSNPs aim to improve health outcomes and reduce administrative burdens, making them a critical option for vulnerable populations seeking a more coordinated and efficient approach to healthcare.

This module equips ProvideSure agents with the skills and strategies to effectively position and sell ancillary insurance products—especially hospital indemnity plans—as essential components of a complete Medicare Advantage solution. Rather than presenting these products as optional add-ons, agents are trained to bundle them confidently and seamlessly into their Medicare consultations. By leading with products like GTL’s Advantage Plus®, agents can normalize cost protection, address common hospitalization concerns, and differentiate themselves as comprehensive advisors rather than transactional sellers. The module emphasizes using emotional storytelling, real cost data, and brand trust to drive client buy-in while introducing key product benefits such as coverage for short hospital stays, ambulance services, skilled nursing, and cancer care. Ultimately, agents learn to present ancillary coverage as the standard for responsible, value-driven Medicare planning.

This module introduces agents to the key differences between Medicare Supplement (Medigap) and Medicare Advantage plans, providing a foundational understanding necessary for effective plan comparisons and client recommendations. Medigap works alongside Original Medicare to cover out-of-pocket costs and allows nationwide provider access without network restrictions, making it ideal for clients who prioritize flexibility and predictability in healthcare expenses. In contrast, Medicare Advantage plans bundle hospital, medical, and often drug coverage into a single plan with lower premiums and added benefits like vision and dental but require use of network providers and may involve referrals. Agents will learn to align plan types with client needs, preferences, and budget, setting the stage for more in-depth exploration and application in future training.

base skills